The alarm on his phone simply labeled “meds” pings as he heads to the Shopper’s Drug Mart where his favourite staff know him by name. For the past three years, Christopher Berger has gone to the same North Edmonton pharmacy, lockbox in hand, to pick up his prescription of Suboxone, a medication used to treat opioid use disorder.
Berger is a client of Alberta Health Services’ Virtual Opioid Dependency Program (VODP) and has been since 2019. The program was established in 2017 and enables clients like Berger to virtually or telephonically access experts who specialize in opioid recovery including physicians, case managers, and counsellors. The program was a necessary response to a body count that continues to rise as a direct result of illicit drug poisoning. According to substance use surveillance data collected by the province, Alberta reported a devastating 1,758 deaths from tainted drug supply in 2021 alone. Berger knows he is one of the lucky ones. “I’ve come close,” he shares. “Those drugs are poison. I’m so thankful that I found the program when I did.”
Access to addiction recovery is an issue as domineering as substance abuse itself. Wait lists for publicly funded care often exceed a six-month period, and that time is something Berger’s VOPD case manager, Jill Sorenson, says people in crisis simply don’t have. ”We are struggling to even get people into detox because the need is overwhelming,” she says. “When a person does get in, they can’t stay until a space opens up in treatment. They are told they’ll be waiting months, usually with an expectation they stay clean. It’s unrealistic, discouraging, and dangerous.“
Berger was referred to VODP after his own brief stay in an Edmonton detoxification facility and remembers his desperation as poignantly as his relief. “I would have done anything at that point,” he recalls. “I don’t think I could have gone much longer without killing myself, either accidentally or on purpose.”

During intake, a case manager assessed his current using patterns, lifestyle, and social commitments to determine what supports and program structure would suit him best. “They asked me everything. I felt a bit like I was being interrogated,” Berger says. VOPD offers weekly virtual counselling services with trained addictions therapists, and this convenient support has been a lifeline for Berger. “My case manager Jill hooked me up with Amber, my therapist, and she is one of the best confidants I’ve ever had. She might not know what it’s like to be addicted to (opioids), but she obviously knows how to care about someone who is.”
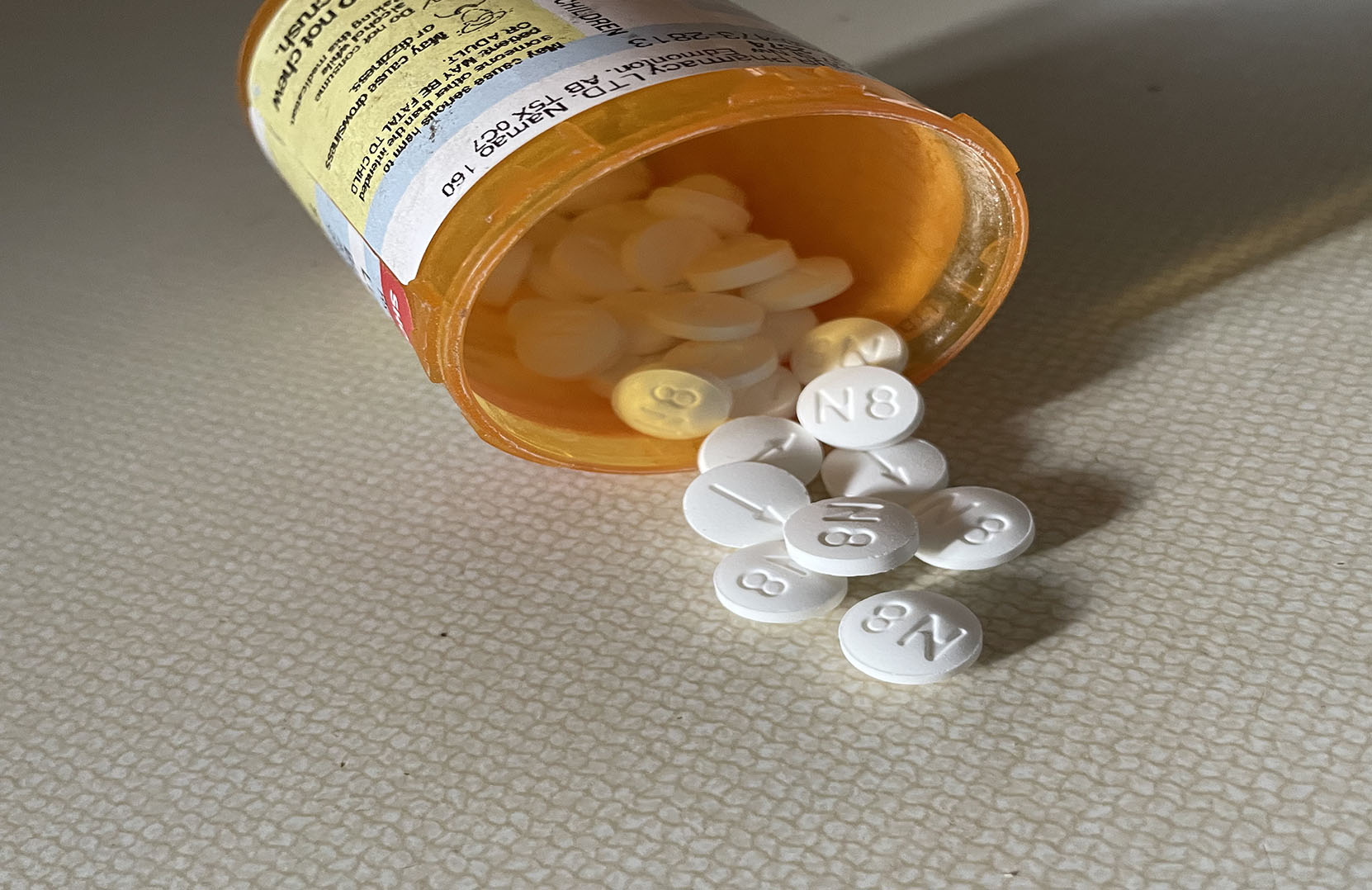
In addition to psychological support, Berger uses a medication that not only relieves symptoms of withdrawal but prevents substance misuse and potential drug poisoning. According to The College of Physicians and Surgeons in Alberta (CPSA), Suboxone is a blend of Buprenorphine, an opioid replacement that prevents symptoms of dope sickness, and Naloxone, a powerful medication that inhibits opioid misuse. Typically, Naloxone is given after a person has overdosed since it can revive them long enough to be transferred to a medical facility, but when taken as Suboxone, an overdose is prevented in the first place. This is a tool Berger insists he literally could not live without. “I didn’t stop using altogether when I first started the program,” Berger admits. “I always overdid it, and I’m sure Suboxone is the only reason I didn’t die.”
Suboxone is not without its controversy. Berger remembers that he hesitated before starting on his medication because of certain stigma and misconceptions regarding these meds, sometimes perpetuated in abstinence-enforcing recovery circles. Sorenson confirms this is a common concern and describes how many prospective clients toil with the concept of taking one drug to replace another. “A perception we hear a lot is that our program and the meds we prescribe is a cop-out or less effective way to quit, but Suboxone is not impairing at all,” she says. She continues that clients who check in with their counsellors and take their meds, regardless of abstinence, have a reported better quality of life. “Of course quitting is the goal, but Suboxone acts as a safety net if a person does relapse. And it helps a person get back to their life without struggling through dope sickness or cravings. Most deaths we see happen after a period of abstinence because a person’s tolerance has lowered. We know a dead client never recovers.”
Berger is proud of the year he has had and grateful to all of the supports who remain a simple phone call away. He recommends that anyone in Alberta who is struggling to reach out immediately. “Just make the phone call,” Berger insists. “Talk to someone who can help. They helped me keep my job and get my family back. I don’t have to fight so hard anymore because this program keeps me out of hell.”
Images: Kaylee Sime



0 Comments